Is It PAWS (Post-Acute Withdrawal)…or Just a Bad Week?
Is it PAWS or just a bad week? Learn how to spot post-acute withdrawal symptoms, understand mood changes in recovery, and know when to seek support.
.png)
Recovery isn’t a straight line. Even after detox or residential treatment, there are days – or weeks – when you feel flat, irritable, anxious, or exhausted for no obvious reason. For people who’ve stopped using alcohol or other drugs, those stretches can raise a frightening question:
“Is this Post-Acute Withdrawal Syndrome… or am I just having a bad week?”
Post-Acute Withdrawal Syndrome (PAWS) refers to psychological and mood-related symptoms that persist for weeks, months, or even years after the acute phase of withdrawal has passed. It’s linked to long-term changes in the brain after chronic substance use and is recognised as a major risk factor for relapse.
At the same time, everyone in recovery still goes through ordinary life stress: tough workdays, conflict at home, grief, financial pressure. Not every slump is PAWS.
This guide walks through what PAWS is, what a “normal” bad week might look like, and how to tell when it’s time to reach out for extra support.
Understanding PAWS
Definition of PAWS
Post-Acute Withdrawal Syndrome (PAWS) describes longer-lasting withdrawal-related symptoms that continue after the initial, physical withdrawal period ends. Instead of lasting days, these symptoms can linger or recur in waves for months to a couple of years, depending on the person and the substance.
PAWS has been reported after withdrawal from a range of substances, including:
- Alcohol
- Opioids (e.g., heroin, prescription pain medications)
- Benzodiazepines and other sedatives
- Stimulants (e.g., cocaine, methamphetamine)
- Cannabis
- In some reports, nicotine, antidepressants, and antipsychotics
While acute withdrawal is usually dominated by physical symptoms (sweats, shakes, nausea), PAWS is more about emotional, cognitive, and energy-related changes that linger as the brain continues to heal.
Timeline:
- Acute withdrawal: typically lasts from a few days up to ~2 weeks, depending on the substance and level of dependence.
- PAWS: symptoms generally begin after acute withdrawal settles and may come and go for several months, and in some cases up to 1–2 years, gradually lessening over time.
Symptoms of PAWS
Common PAWS symptoms include:
- Mood changes
- Depression or low mood
- Irritability, anger, or emotional overreactions
- Feeling “numb” or detached
- Anxiety
- A sense of restlessness, worry, or unease
- Panic-like feelings without a clear trigger
- Fatigue and low motivation
- Feeling drained even with adequate sleep
- Difficulty starting or completing tasks
- Sleep disturbances
- Insomnia or broken sleep
- Vivid or disturbing dreams
- Cognitive challenges
- “Brain fog” – trouble concentrating or thinking clearly
- Short-term memory problems
- Slowed thinking
One hallmark of PAWS is that these symptoms often fluctuate. You might have a stretch of feeling almost back to normal, followed by a few rough days where symptoms surge, even though nothing obvious has changed. Many people describe this as a “wave” pattern rather than a constant state.
Physiological and Psychological Factors
PAWS isn’t “all in your head.” It reflects real, ongoing changes in brain chemistry after chronic substance use and withdrawal.
Chronic use of substances like alcohol, opioids, and benzodiazepines leads to neuroadaptations – the brain adjusts to the constant presence of these chemicals by changing how it releases and responds to neurotransmitters (such as GABA, glutamate, dopamine, and stress-related hormones).
When the substance is removed, the brain has to gradually rebalance. During this period, people may experience:
- Dysregulated stress responses (feeling “on edge” or overwhelmed)
- Mood instability (swings between low mood and irritability)
- Changes in reward and motivation (reduced ability to feel pleasure, low drive)
On the psychological side, PAWS often overlaps with:
- Grieving the loss of substances that were used to cope with emotions
- Facing unresolved trauma, relationship issues, or life stress without numbing
- Adjusting to new routines and identities in early recovery
In other words, PAWS is usually a blend of brain healing and emotional adjustment, which can make it confusing to untangle.
Recognizing a Bad Week
Not every rough patch means PAWS. Sometimes, life is simply hard – even when recovery is going well.
What Constitutes a Bad Week?
A “bad week” might include:
- Work stress (deadlines, conflicts, job insecurity)
- Strain in relationships (arguments, breakups, family tension)
- Health issues or poor sleep for a few nights
- Financial worries, childcare challenges, or other life changes
In these cases, your mood and energy take a hit, but the stressor is usually clear: you can point to what changed. Feeling low or overwhelmed in response to real-life stress is normal, even in stable long-term recovery.
Signs It’s Just a Bad Week
While only a professional can fully assess your situation, some signs that you might be having a tough week rather than PAWS include:
- Clear triggers
- You can link how you feel to specific events (a stressful meeting, bad news, conflict with a partner).
- Shorter duration
- Symptoms ease as the stressor resolves or as you use healthy coping skills over several days.
- Less wave-like pattern
- Feelings are more closely tied to circumstances than random “out of nowhere” dips weeks into sobriety.
- Functioning is strained, but intact
- You may feel off, but you can still go to work, attend meetings, and manage basic responsibilities most of the time.
- Healthy coping helps
- Basic strategies – sleep, exercise, talking with a friend or therapist, using your recovery tools – bring noticeable relief.
Even “just” a bad week deserves care. It’s still important to lean on support, protect your recovery, and watch for any intensifying signs that might call for professional input.
Distinguishing Between PAWS and a Bad Week
Key Differences
The table below highlights some general differences. These are not strict rules, but they can help you think about what you’re experiencing:
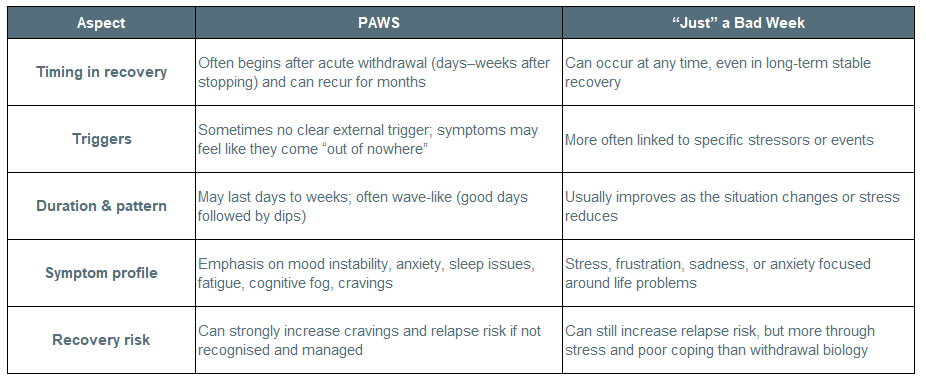
Remember: PAWS and bad weeks can overlap. You might have a PAWS wave during a stressful time, which can make everything feel more intense.
Clinician Perspective
One of the most destabilizing parts of early and mid-recovery isn’t the symptoms themselves, it’s the meaning people attach to them. I regularly see clients panic when a low mood, irritability, or foggy thinking shows up weeks or months after stopping substances. The thought quickly becomes, “Something is wrong with me,” or “I should be past this by now.” That fear can be more dangerous than the symptoms.
From a clinical standpoint, PAWS and “bad weeks” exist on a continuum rather than in neat boxes. Brain healing does not follow a calendar, and life stress does not pause just because someone is sober. What matters most is pattern recognition over time, not a single rough stretch. When symptoms come in waves, feel disproportionate to circumstances, or begin to erode confidence in recovery, that’s a signal to slow down and add support, not a sign of failure.
I also want to normalize this: having a bad week in recovery does not mean you are regressing. In fact, learning to tolerate emotional discomfort without numbing is often evidence that recovery is working. The goal is not to feel good all the time. The goal is to stay connected, curious, and supported when you don’t.
When clients shift from asking “What’s wrong with me?” to “What does my nervous system need right now?” they tend to move through both PAWS and ordinary life stress with far less shame and far more resilience. And that mindset, more than any single diagnosis, is what protects long-term recovery.
Dr. Nicole Erkfitz, LCSW
Chief Operating Officer, Mainspring Recovery
Seeking Professional Help
You should consider talking with a healthcare or addiction professional if:
- Your symptoms are strong, persistent, or worsening over several weeks.
- You’re experiencing severe depression, intense anxiety, or panic that doesn’t ease with basic coping.
- You notice strong cravings or thoughts of using, especially if they feel hard to resist.
- Your sleep, appetite, or ability to function day to day is significantly disrupted.
- You’re unsure whether what you’re experiencing is PAWS, a mood/anxiety disorder, or something else.
A clinician familiar with addiction and recovery can:
- Review your substance use history, timeline of symptoms, and current supports.
- Help differentiate PAWS from other mental health conditions.
- Adjust your treatment plan – for example, changing medications, recommending therapy modalities, or suggesting a higher or lower level of care.
If you’re having thoughts of self-harm or suicide, or feel unsafe, it’s important to seek help immediately. In the United States, you can call or text 988 to reach the Suicide & Crisis Lifeline 24/7.
Coping Strategies and Resources
Managing PAWS Symptoms
The most important message about PAWS is that it is real, and it is usually temporary. These symptoms reflect the brain’s ongoing adjustment and can be managed with the right supports.
Helpful strategies include:
- Stay connected to treatment and support
- Continue with individual therapy, group therapy, or Intensive Outpatient / Virtual IOP if recommended.
- Attend peer-support meetings (12-step, SMART Recovery, or other groups).
- Use structure and routine
- Keep regular sleep and wake times.
- Maintain a predictable daily schedule with small, achievable tasks.
- Support your body
- Aim for consistent sleep hygiene (limit caffeine late in the day, build a wind-down routine).
- Eat regular, balanced meals and drink enough water.
- Incorporate gentle movement (walking, stretching, yoga) most days.
- Practice emotional regulation skills
- Mindfulness or grounding exercises when anxiety spikes.
- Journaling to track patterns in mood, sleep, and cravings.
- Cognitive-behavioural techniques (identifying and challenging unhelpful thoughts).
- Have a relapse-prevention plan ready
- Identify early warning signs (isolation, romanticising substance use, skipping supports).
- Keep a list of people and services you can contact when urges or symptoms surge.
For family members and caregivers:
- Learn about PAWS so mood swings and fatigue are less confusing.
- Offer consistent, calm support rather than pressure or criticism.
- Encourage your loved one to keep appointments and use coping tools.
- Take care of your own mental health through therapy, groups, or respite when needed.
Navigating Bad Weeks
When your struggles are more clearly related to life stress than withdrawal, many of the same tools still apply:
- Name the stressors
- Identify what’s weighing on you (work, relationships, health) rather than pressuring yourself to “snap out of it.”
- Adjust expectations
- In a hard week, prioritise essentials: staying sober, meeting key responsibilities, and basic self-care. It’s okay to postpone non-urgent tasks.
- Lean on your support system
- Talk honestly with trusted friends, family, sponsors, or therapists.
- Let people know what you need – listening, problem-solving, or simply company.
- Use healthy stress-relief
- Relaxation practices (deep breathing, progressive muscle relaxation, short walks).
- Limiting doom-scrolling and alcohol- or drug-related content.
- Know when to escalate support
- If a “bad week” starts to stretch into multiple weeks, or your symptoms intensify, treat that as a sign to reach out for professional guidance rather than trying to “tough it out” alone.
How Mainspring Recovery Supports People Living With PAWS
At Mainspring Recovery in Virginia, PAWS is recognised as a real and challenging part of many people’s recovery journeys. The team provides a full continuum of care – from medical detox and residential treatment to Partial Hospitalization (PHP) and Intensive Outpatient (IOP) levels – so support doesn’t stop when acute withdrawal ends.
Because PAWS symptoms can come in waves and often show up after someone has returned home, structured programs like PHP and IOP are designed to:
- Teach practical skills for managing mood swings, anxiety, and cravings
- Provide regular check-ins with clinicians who understand PAWS and relapse risk
- Create a safe space to talk through “bad weeks,” whether they’re driven by brain chemistry, life stress, or both
If you’re not sure whether what you’re feeling is PAWS or just a rough patch, talking with a team that works with these patterns every day can bring clarity – and relief.
Conclusion
In early and middle recovery, it’s completely understandable to wonder:
- “Is this PAWS?”
- “Am I slipping backwards?”
- “Or is this just a hard week like anyone can have?”
PAWS involves ongoing, often wave-like symptoms – mood changes, anxiety, fatigue, sleep and thinking problems – that show up after acute withdrawal and can last for months as the brain recalibrates. Bad weeks are a normal part of life, usually tied to clear stressors and shorter in duration.
Both deserve attention. Both can affect your recovery. And both are easier to navigate with support.
The most important step is not to diagnose yourself but to stay curious, honest, and connected:
- Notice your patterns and triggers.
- Use the coping strategies that support your body, mind, and sobriety.
- Reach out to professionals when symptoms are intense, confusing, or persistent.
You don’t have to decide alone whether it’s PAWS or just a bad week. With the right treatment team and support network, you can move through both and keep building a stable, sustainable recovery.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical or mental health advice, diagnosis, or treatment. Always speak with a qualified healthcare provider about your individual situation, especially if you are in crisis, thinking about harming yourself, or worried about relapse.
Sources:
https://pubmed.ncbi.nlm.nih.gov/36731102/
https://www.ncbi.nlm.nih.gov/books/NBK459239/
https://library.samhsa.gov/sites/default/files/sma10-4554.pdf)
https://americanaddictioncenters.org/withdrawal-timelines-treatments/post-acute-withdrawal-syndrome
https://www.addictioncenter.com/treatment/post-acute-withdrawal-syndrome-paws/
Related articles

How to Build Financial Independence in Sobriety

The Importance of Continuing Education on Addiction Recovery

How to Recognize the Signs of Addiction

How Substance Abuse Impacts Physical Fitness

The Benefits of Developing a Healthy Routine During Recovery
Welcome to Mainspring Recovery, The #1 Rehab Center in Virginia
You don’t have to walk the road to recovery alone. At Mainspring Recovery, we know how important it is to have a trusted partner while you leave drugs and alcohol behind. Find a brighter tomorrow by starting with our compassionate team of medical professionals and recovery specialists today at our rehab center in Virginia.
Call: 571-583-5115
Fax: 571-749-9420
Email: admissions@mainspringrecovery.com
Emailfor all records requests: medicalrecordsdumfries@mainspringrecovery.com

